Our Vision
We envision an America where all individuals, families, and communities have access to culturally preferred, nutritious food to help prevent, manage, and treat diet-related diseases and promote health and well-being.
Our Food Is Medicine (FIM) work is grounded by the understanding that:
- Access to nutritious food is critical to health and resilience.
- Healthy eating patterns can reduce the risk of many diseases and health conditions.
- Healthy eating patterns play an important role in physical development; maintenance of healthy skin, teeth, and eyes; bone strength; muscle and digestive function; and immunity; and contribute to improved quality of life.
Achieving this vision will require a whole-of-government and whole-of-society approach that ensures the healthy choices are the easy choices.
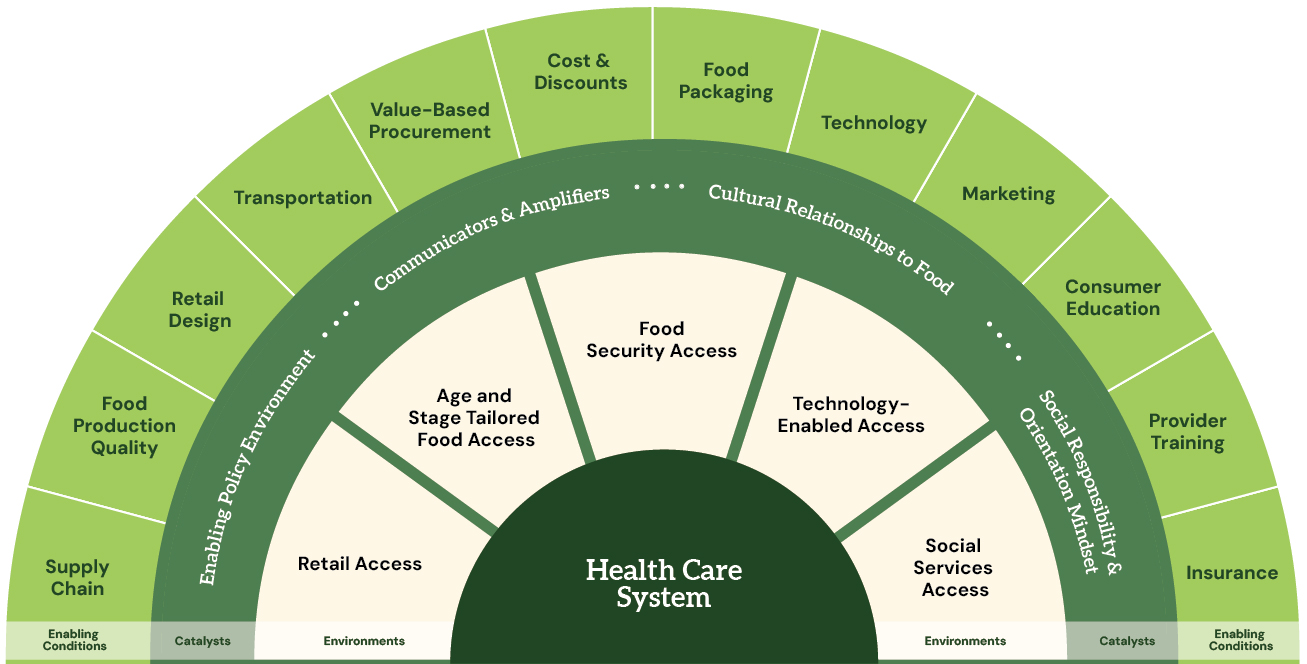
The graphic below illustrates the FIM ecosystem and its many relevant components. An integrated system will support an infrastructure of FIM providers and pathways to access that can help local governments, agencies, and organizations meet the increased demand for healthy food options.
Food Is Medicine Opportunities
We need transformative programs, policies, and system changes within and outside the government. There is no simple solution to these complex issues.
The success of FIM interventions requires strong collaboration between health care, community-based organizations (CBOs), food producers and retailers, and public sector partners. We must work together to encourage the integration of Food Is Medicine interventions across communities and systems.
We have already witnessed strong effort and investment across several systems and organizations. Many organizations are advancing Food Is Medicine efforts and seeking partnership with federal agencies to collaboratively address growing need where diet and health care intersect.
When leaders integrate interventions in their organizations, they can better assist their participants in following dietary recommendations by directly increasing the affordability and accessibility of culturally relevant, healthy foods and enabling sustained dietary changes.
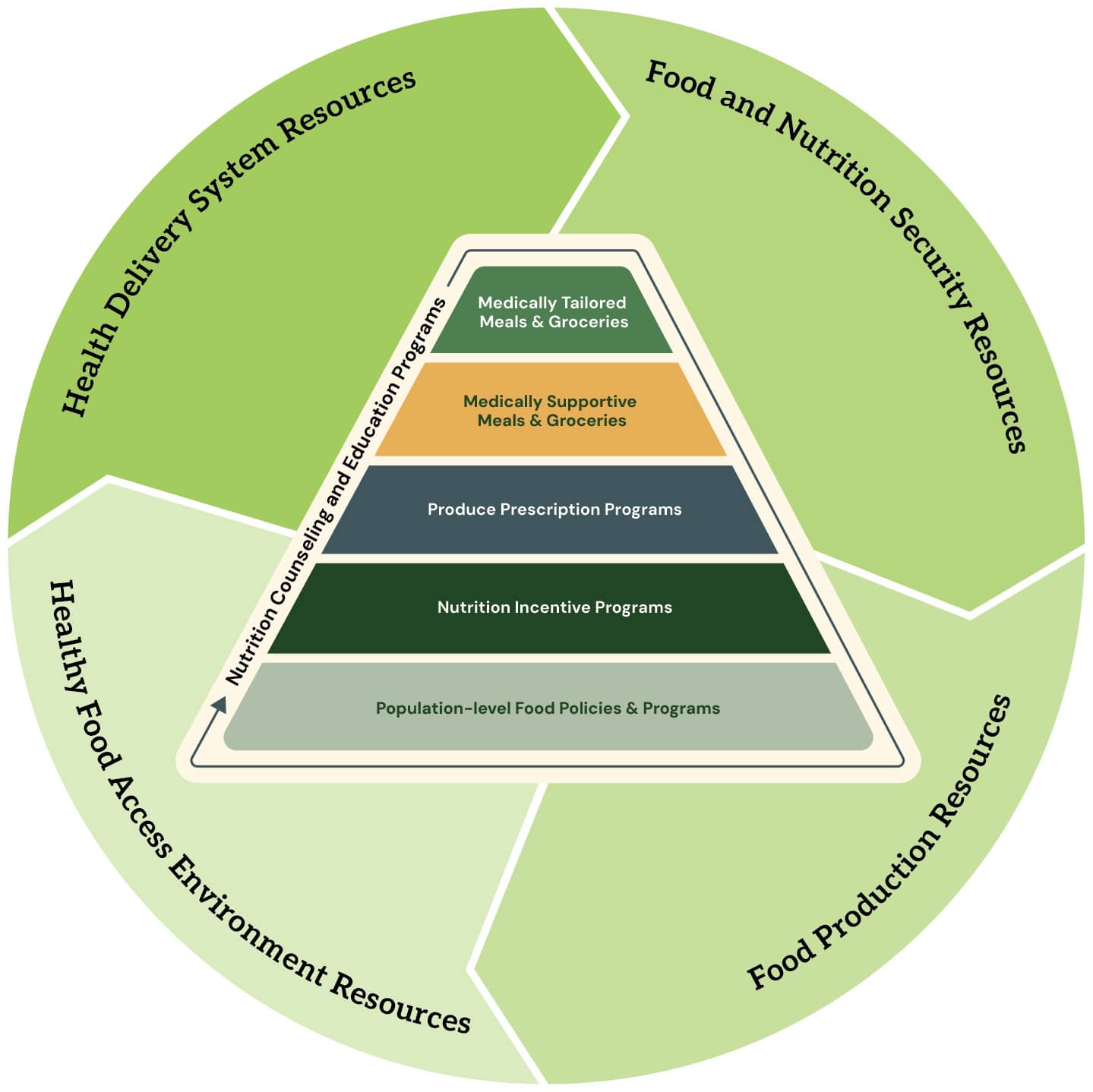
The graphic below represents a holistic federal perspective of FIM interventions and enabling qualities and resources. Central to FIM are the specific interventions that are implemented at the nexus of health care and community systems. These include a range of approaches that support a continuum of need, from acute to prevention. FIM program models include medically tailored meals and groceries, medically supportive meals and groceries, produce prescription programs, and nutrition incentive programs. FIM program models are provided in partnerships with nutrition counseling and education resources that are tailored to the intervention’s structure. Population-level food policies and programs are included at the base of the pyramid because these actions directly support FIM interventions within community structures to enable greater individual health benefit.
The graphic also illustrates how FIM program models are situated at the intersection of broader systems that are complementary to, but distinct from, FIM program models. Surrounding the pyramid are key FIM-enabling systems: health delivery system resources, food and nutrition security resources, healthy food access environment resources, and food production resources.
Food Is Medicine Initiative Timeline
In September 2022, the White House issued a National Strategy on Hunger, Nutrition, and Health to end hunger and reduce the burden of diet-related diseases by 2030. Through this strategy, we established the “Food Is Medicine Initiative to Unify and Advance Collective Action.” This strategy includes diet-related research and programmatic efforts that will increase access to Food Is Medicine initiatives.
Federal Food Is Medicine Collaborative
Federal government colleagues who support Food Is Medicine solutions participate in the Federal Food Is Medicine Collaborative. This group works to establish a shared vision and common language for a unified federal Food Is Medicine effort.
The collaborative is the first and only interdepartmental initiative to include federal departments directly supporting Food Is Medicine interventions and the systems supporting these programs.
The group works to advance Food Is Medicine by:
- Providing thought partnership and leadership to build an aligned federal understanding and approach.
- Engaging in learning and synthesis of best practices and needs to advance Food Is Medicine programs and investments.
- Building collaborative action that can support policy and practice across the federal government and the nation.
The graphic below describes the 4 key opportunities that the Federal Food Is Medicine Collaborative identified for federal action to advance Food Is Medicine.